Understanding the difference between osteoarthritis and arthritis is essential for accurate diagnosis and appropriate treatment. Although these two terms are often used interchangeably, they denote distinct conditions affecting the joints.”
Osteoarthritis
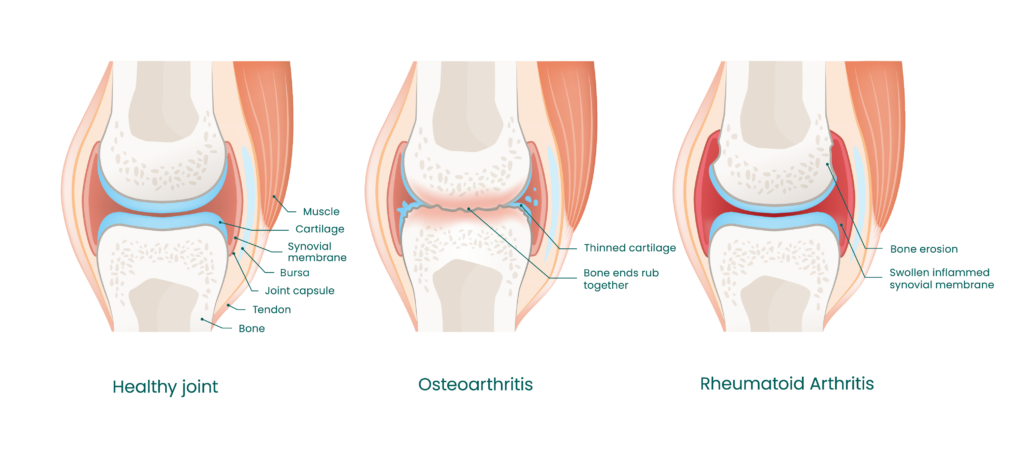
Osteoarthritis is the most common form of joint disease, primarily linked to aging and wear of the joints. This degenerative disease affects the cartilage, a smooth, protective substance covering the ends of bones within a joint. As the cartilage wears away, bones begin to rub against each other, causing pain, stiffness, and loss of movement.
What are the causes of osteoarthritis?
The causes of osteoarthritis are varied: aging, joint trauma, genetics, obesity, and overuse of joints are the main factors.
- Aging increases the risk of osteoarthritis, as natural wear on the joints can degrade cartilage.
- Injuries, whether acute such as a fracture, or repetitive such as microtraumas linked to certain sports, can damage cartilage and accelerate the development of osteoarthritis.
- Genetic predisposition can also play a role.
- Excess weight puts additional pressure on weight-bearing joints such as the knees and hips, accelerating cartilage wear.
- Finally, professions or hobbies involving repetitive movements can increase the risk of osteoarthritis by causing excessive joint wear.
Symptoms of osteoarthritis
Symptoms of osteoarthritis typically develop slowly and get worse over time. They include joint pain, stiffness, loss of flexibility, a sensation of grinding during movement, and the formation of bone spurs (osteophytes).
Pain is often felt during movement or after a period of inactivity, while stiffness is most noticeable in the morning or after a period of rest.
The diagnosis is based on a clinical examination, X-rays, and laboratory tests to exclude other causes of joint pain.
- During the clinical examination, the doctor will inspect the joints for signs of pain, swelling, stiffness, and deformity, assessing joint mobility and pain experienced during movement.
- X-rays can reveal loss of cartilage, bone spurs, and narrowing of the joint space.
- Sometimes, additional imaging tests may be requested to further specify the diagnosis.
- While blood tests cannot diagnose osteoarthritis, they can help to exclude other causes of joint pain, such as infections or inflammatory diseases.
Treatments for osteoarthritis
There is no cure for osteoarthritis, but several treatments can help manage symptoms.
- Medications include pain relievers such as acetaminophen, or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen to reduce pain and inflammation.
- Corticosteroid injections can help temporarily relieve pain and inflammation.
- Physiotherapy, including exercises to strengthen muscles around the joints, improve flexibility, and reduce pain, is often recommended.
- Aquatic therapy can also contribute to symptom improvement.
- Reducing body weight can also help decrease pressure on weight-bearing joints. Using assistive devices such as braces, canes, or supportive footwear can reduce the load on affected joints.
- In severe cases, joint replacement surgery, such as hip or knee prosthesis, may be necessary to improve joint function and reduce pain.
Arthritis
Arthritis, on the other hand, is a generic term referring to over 100 different types of inflammatory joint diseases. Unlike osteoarthritis, which is a degenerative disease, arthritis involves inflammation of the joints and can affect people of any age.
Different types of arthritis
Common types of arthritis include rheumatoid arthritis, psoriatic arthritis, gout, and juvenile arthritis.
- Rheumatoid arthritis is an autoimmune disease where the immune system attacks the synovial membrane, causing inflammation and joint destruction.
- Psoriatic arthritis, associated with psoriasis, causes joint inflammation and skin rashes.
- Gout is a form of arthritis caused by the accumulation of uric acid crystals in the joints, leading to acute inflammation.
- Juvenile arthritis affects children and results in joint inflammation.
What are the causes of arthritis?
The causes of arthritis vary depending on the type, but may include genetic factors, infections, autoimmune responses, and crystal deposits.
- Hereditary predisposition may play a role in certain forms of arthritis, with specific genes making some individuals more likely to develop these conditions.
- Some viral or bacterial infections can trigger an inflammatory response in the joints.
- In diseases like rheumatoid arthritis, the immune system mistakenly attacks joint tissues.
- Lastly, crystal deposits (such as uric acid or calcium pyrophosphate) can cause acute and painful joint inflammation.
Symptoms of arthritis
Symptoms of arthritis also vary by type, but often include joint pain, swelling, stiffness, redness, and fatigue.
- Pain can be constant or intermittent and affect one or multiple joints. Diagnosing arthritis requires a thorough examination including physical examination, laboratory tests, and imaging.
- A doctor will look for signs of swelling, redness, warmth, and deformity in the joints, also assessing joint mobility and pain.
- Blood tests can detect inflammatory markers, rheumatoid factors, or specific antibodies.
- Analysis of synovial fluid (fluid within the joints) may also be performed to detect infections or crystals.
- X-rays and other imaging modalities allow observation of joint damage, bone erosion, and structural changes.
Treatments for arthritis
Treatments for arthritis aim to reduce symptoms and improve quality of life. Treatments can vary depending on the final diagnosis, but may include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation;
- Corticosteroids for rapid inflammation reduction, administered orally or by injection;
- Disease-modifying antirheumatic drugs (DMARDs) such as methotrexate and sulfasalazine to slow disease progression;
- Biologic medications that target specific components of the immune system (such as TNF inhibitors) to treat severe forms of autoimmune arthritis.
Physiotherapy, including exercises to maintain joint mobility and strength, as well as techniques to reduce pain, is often recommended. Lifestyle changes, such as specific diets (for example, a low-purine diet for gout), stress management, and modifications to activities to reduce joint pressure, can also be beneficial.
In severe cases, surgical interventions such as synovectomy (removal of inflamed synovial membrane) or joint replacement may be necessary.
In conclusion, although osteoarthritis and arthritis both affect the joints, their causes, symptoms, and treatments differ significantly. Accurate diagnosis and a clear understanding of these differences are essential for effectively managing each condition and improving patients’ quality of life. If you experience joint symptoms, it’s important to consult a healthcare professional for an accurate diagnosis and tailored treatment plan.