The incidence of colon cancer
The incidence and mortality rate of colon cancer varies significantly from one place to another in the world. According to the World Health Organization, colon cancer is the third most frequently diagnosed cancer in men and the second in women. Each year, approximately 6,000 new cases are diagnosed in Quebec. Since the mid-1980s, mortality rates due to colorectal cancer have gradually decreased. This improvement can be attributed in part to the detection and resection of colonic polyps, the detection of colorectal cancers at an earlier stage, and more effective primary and adjuvant treatments.
In North America, the lifetime incidence in an average-risk person is approximately 4%. Age is a major risk factor for sporadic colorectal cancer. Colorectal cancer is rare before the age of 40; Incidence begins to increase significantly between the ages of 40 and 50, and age-specific incidence rates increase with each subsequent decade. Age is therefore a factor that influences colorectal cancer screening recommendations.
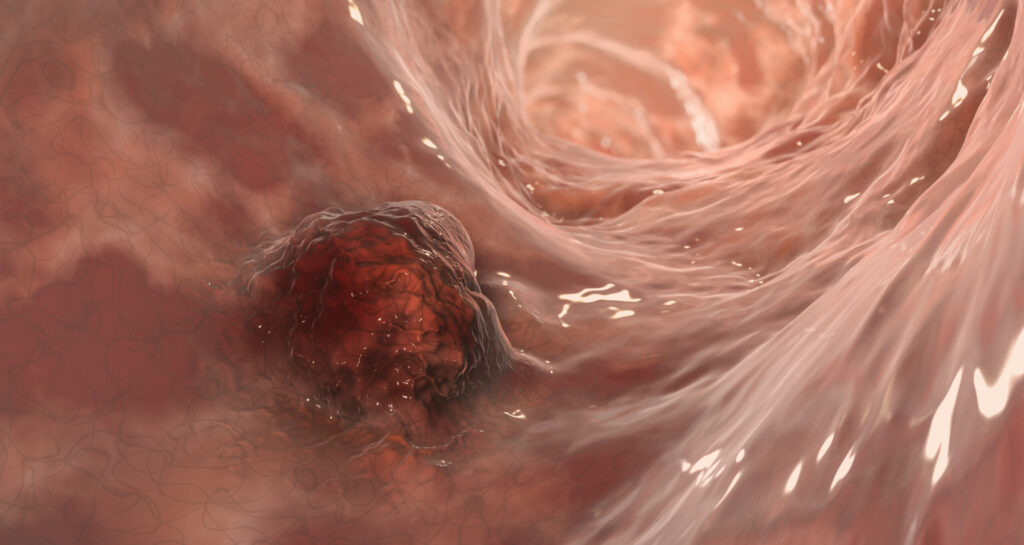
Colon cancer develops from the lining of the colon, the inner layer of the large intestine wall. The process begins with the formation of polyps. Not all polyps become cancerous, but almost all colorectal cancers begin as an adenomatous polyp. As the polyp grows, cellular changes called dysplasia can occur. Dysplasia is a pre-cancerous condition where cells in the lining become abnormal, but not yet cancerous. If the dysplastic cells continue to accumulate genetic mutations, they can become cancerous, forming an adenocarcinoma. This means that the cancer cells multiply out of control and invade the lining of the colon. This whole process occurs over a period of about ten years. Hence the importance of adhering to regular screening.
The screening
In most individuals, screening is done by an immunochemical test for fecal occult blood (iFOBT). This is a non invasive test that detects the presence of blood in the stool, a potential sign of colon cancer or precancerous polyps. This test is recommended for asymptomatic people aged 50 to 74, every two years. In people with a positive iFOBT test, a coloscopy is recommended. This method will visualize the entire colon, assess the possible origin of the bleeding, remove polyps or perform biopsies in a single procedure.
In individuals at higher risk of colorectal cancer than the general population, the iFOBT could be recommended from the age of 40 or a coloscopy could be recommended immediately. These factors that influence the age at which screening begins and the method chosen are the presence of: hereditary colon cancer syndromes, personal or family history of colorectal cancer or precancerous polyps, inflammatory bowel disease, and past exposure to abdominal radiation therapy.
Which factors increase the risk of colon cancer?
Several lifestyle factors are associated with an increased risk of colorectal cancer. Although many of these associations have been observed very consistently in observational studies, the causal relationship of these associations is not always proven. The population should still be encouraged to reduce or avoid these factors for the prevention of colorectal cancer.
- Weight management: Studies have reported that weight gain between early adulthood and middle age was associated with a modest but significant increase in the risk of colorectal cancer.
- Diabetes and insulin resistance: One possible explanation linking diabetes to colorectal cancer is hyperinsulinemia, as insulin is an important growth factor for colonic mucosal cells and stimulates colonic tumor cells.
- Red and processed meats: Their long-term consumption appears to be associated with an increased risk of colorectal cancer. High-temperature cooking (BBQ, pan-frying) has been implicated as contributing to the risk.
- Tobacco: It is associated with a higher incidence and mortality of colorectal cancer. It is also a risk factor for all types of colonic polyps.
- Alcohol consumption: The risk increases with at least moderate consumption, i.e. more than 2 to 3 drinks per day.
Several protective factors have also been identified, mainly in observational studies, but the strength of some of these associations is uncertain. In particular, regular physical activity and a diet rich in fruits and vegetables.
- Calcium and vitamin D supplementation appears to have a protective effect on colorectal cancer, but studies are sometimes contradictory.
- Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) can protect against the development of colonic adenomas and are associated with a reduced long-term risk of colorectal cancer. However, in the absence of other indications for the use of these molecules, they are not used to prevent the development of colorectal cancer in the general population.
How to prevent colon cancer?
Having good lifestyle habits and individualizing screening according to non-modifiable risk factors are good practices for preventing and detecting colorectal cancer. Do not hesitate to discuss this with your healthcare professional.