Lipoprotein(a), commonly known as Lp(a), has been rapidly rising up the ranks as a compelling biomarker for assessing cardiac risk in the past years. Encoded by the LPA gene, Lp(a) is a form of low-density lipoprotein (LDL). It is the single highest, genetically inherited trait that can give you a high risk of developing Atherosclerotic Cardiovascular Disease (ASCVD). Close to 20% of the population have elevated Lp(a), sitting in the category of high risk patients. It’s not 100% deterministic though, there are many other factors contributing to ASCVD, not everyone with high levels of Lp(a) will develop the disease.
In a nutshell, the gene LPA codes for an apolipoprotein a. This apo(a) will then bind to an apoB on an LDL. That combinaison of apo(a) + apoB on/around a LDL is what we call a Lp(a) particle. This modified LDL is more atherogenic and unfortunately, satins, a common LDL lowering drug class, will not work to lower this modified version of it.
Lp(a) and Cardiac Risk Stratification: Proven Validity based on Robust Data
The role of Lipoprotein(a) (Lp(a)) in assessing cardiac risk has been reinforced by recent genetic evidence demonstrating a strong association of high Lp(a) levels with enhanced risk of ASCVD and calcific aortic valvular disease (CAVD). Lp(a) levels, which are largely genetically determined, have shown a strong correlation with ASCVD. We have 3 solid studies publish in 2009 showing that people with variant associated with elevated Lp(a) also have more cardiovascular events.
Now, what are the normal levels and what does it mean in the context of developing ASCVD?
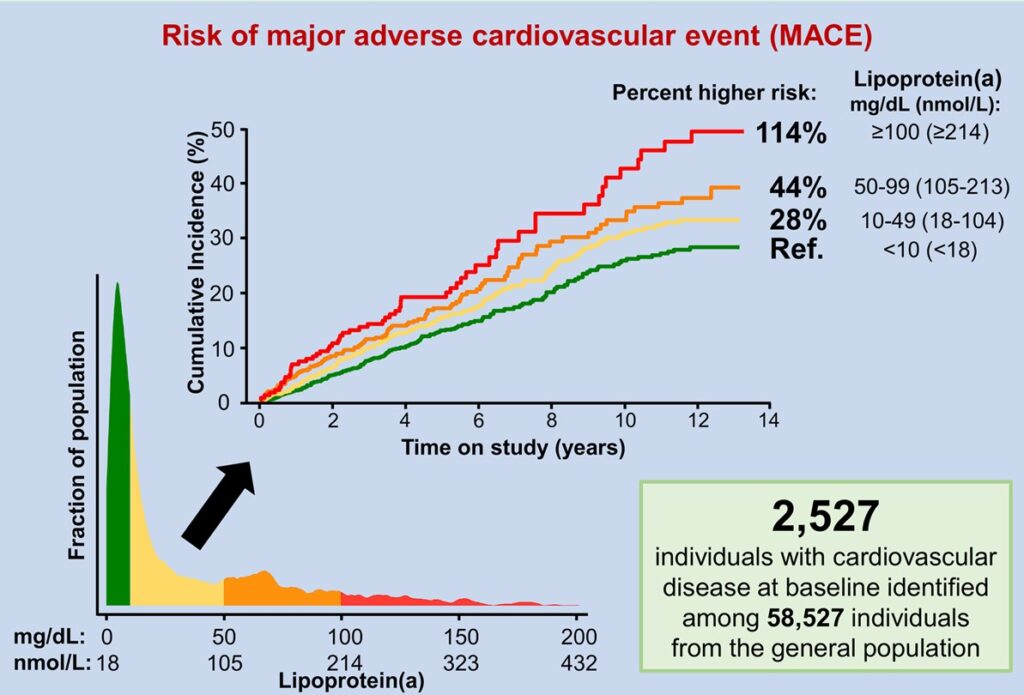
As you can appreciate in this figure, normal risk is defined as where the bulk of the population stands, i.e, at or below 18 nmol/L. Then, we define 3 additional categories of risk of Major Adverse Cardiovascular Event (MACE). MACE include for example: death from a cardiovascular event, myocardial infarction, stroke, hospitalization for heart failure, etc. Bad stuff.
Now, let’s not panic at the color schemes and percent higher risk values here. Those are relative risks, which means comparing the percentages increase in the group above, to the group below.
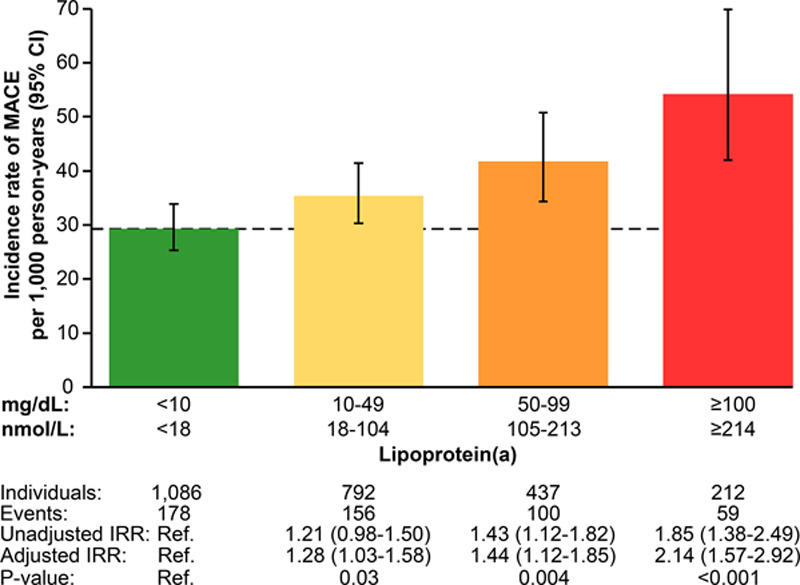
When calculated in absolute risk, we see a baseline of 29 MACE per 1000 person-years jump to 59 for the highest risk group. It’s less impressive than stating a 114% risk increase, but it is a lot, especially when considering the severity of what a MACE is.
What does it mean in practice?
It simply means we have another tool to assess the risk of an individual, along with mainly (but not exclusively) apoB, non-HDL cholesterol and LDL-C. The Canadian Cardiovascular Society guidelines emphasize that Lp(a) levels should be measured once in a person’s lifetime (for now, or until we have new treatments that reduce this value significantly).
Since I am mostly interested in keeping people healthy and minimizing their lifetime risk of developing chronic diseases such as ASCVD, Lp(a) will help dictate how aggressively I will screen for the disease (using diagnostic modalities) and/or manage the lipids of an individual.
For example, if I have a 40 years old adult, with some excess visceral adipose tissue and an elevated apoB and Lp(a), I will work hard with this patient for early and aggressive lifestyle modifications and consider pharmacological interventions sooner than later, the goal being to delay as much possible the onset of ASCVD.
The way forward
Ensuring appropriate cardiac risk stratification is critical to improving the health outcomes of the population. The emerging data on Lp(a) is promising in augmenting our cardiac risk assessment tools.
In an era of individualized patient care, understanding factors like Lp(a) ensure we move in the right direction: not just to treat disease, but also to predict and prevent it. Canada is leading the way in integrating Lp(a) into practice guidelines. Encouragingly, as medical science continues to evolve, so too does our understanding of the complex interplay between genetics, lifestyle, and the onset of cardiovascular disease.
It is about time we start moving away from the classical 5 and 10 years risk-estimation for heart attacks and use as much information possible to properly assess and manage preemptively the individual risk of ASCVD.
References
- Lipoprotein(a)-Lowering by 50 mg/dL (105 nmol/L) May Be Needed to Reduce Cardiovascular Disease 20% in Secondary Prevention
- Lipoprotein(a): A Genetically Determined, Causal, and Prevalent Risk Factor for Atherosclerotic Cardiovascular Disease: A Scientific Statement From the American Heart Association
- Lipoprotein(a) Concentration and the Risk of Coronary Heart Disease, Stroke, and Nonvascular Mortality
- Oxidation-Specific Biomarkers, Lipoprotein(a), and Risk of Fatal and Nonfatal Coronary Events
- Genetic Variants Associated with Lp(a) Lipoprotein Level and Coronary Disease